Super User
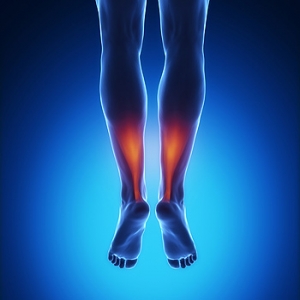
Where Is the Achilles Tendon Located?
 The medical term for the Achilles tendon is the calcaneal tendon. It is located in the back of the leg, and connects the calf muscles to the heel. It is considered to be one of the longest tendons in the body, and is used during walking and running activities. An injury to the Achilles tendon may occur as a result of not warming up adequately before beginning an exercise program. Achilles tendonitis or a rupture can cause severe pain and discomfort. Patients may be susceptible to experiencing this type of injury with existing flat feet or tight calf muscles. There are prevention techniques that can be implemented which may help to reduce the risk of incurring an Achilles tendon injury. These can include stretching before any type of exercise is pursued, in addition to wearing shoes that fit correctly. If you have pain in your heel or if your calf muscles are stiff, please consult with a podiatrist who can properly diagnose and treat Achilles tendon injuries.
The medical term for the Achilles tendon is the calcaneal tendon. It is located in the back of the leg, and connects the calf muscles to the heel. It is considered to be one of the longest tendons in the body, and is used during walking and running activities. An injury to the Achilles tendon may occur as a result of not warming up adequately before beginning an exercise program. Achilles tendonitis or a rupture can cause severe pain and discomfort. Patients may be susceptible to experiencing this type of injury with existing flat feet or tight calf muscles. There are prevention techniques that can be implemented which may help to reduce the risk of incurring an Achilles tendon injury. These can include stretching before any type of exercise is pursued, in addition to wearing shoes that fit correctly. If you have pain in your heel or if your calf muscles are stiff, please consult with a podiatrist who can properly diagnose and treat Achilles tendon injuries.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. John Branwell of Kearny, New Jersey. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Kearny, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Do I Have an Ankle Sprain?
 Unlike a strain, which is an injury to muscle or tendon tissue, a sprain occurs when there is an injury to a ligament. Ankle sprains can be categorized as being Grade 1, Grade 2, or Grade 3. A Grade 1 sprain means the fibers of a ligament have been stretched, not torn, whereas a Grade 2 sprain means the ligament has been partially torn. Grade 3 sprains are described as an injury that causes a ligament to completely tear or rupture. Common symptoms of an ankle sprain include bruising, pain, and swelling of the affected area. For a proper diagnosis and information on how to treat a sprain, please consult with a podiatrist.
Unlike a strain, which is an injury to muscle or tendon tissue, a sprain occurs when there is an injury to a ligament. Ankle sprains can be categorized as being Grade 1, Grade 2, or Grade 3. A Grade 1 sprain means the fibers of a ligament have been stretched, not torn, whereas a Grade 2 sprain means the ligament has been partially torn. Grade 3 sprains are described as an injury that causes a ligament to completely tear or rupture. Common symptoms of an ankle sprain include bruising, pain, and swelling of the affected area. For a proper diagnosis and information on how to treat a sprain, please consult with a podiatrist.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact Dr. John Branwell from Kearny, New Jersey. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our office located in Kearny, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Why Are My Heels Cracking?
 Cracked heels are an uncomfortable, and often painful foot condition. When the cracks of the heel are extremely deep they can be referred to as fissures. Cracked heels can be identified by looking for dry, cracked skin, which can also become discolored to a yellow or brownish shade. If left untreated fissures can worsen over time, becoming more painful and affecting how you walk and go about your normal day to day activities. Cracked heels may develop due to obesity, frequently standing on hard surfaces, the humidity level of your living environment, and skin conditions such as dermatitis or psoriasis. For more information on how to treat cracked heels, it is recommended to consult with a podiatrist.
Cracked heels are an uncomfortable, and often painful foot condition. When the cracks of the heel are extremely deep they can be referred to as fissures. Cracked heels can be identified by looking for dry, cracked skin, which can also become discolored to a yellow or brownish shade. If left untreated fissures can worsen over time, becoming more painful and affecting how you walk and go about your normal day to day activities. Cracked heels may develop due to obesity, frequently standing on hard surfaces, the humidity level of your living environment, and skin conditions such as dermatitis or psoriasis. For more information on how to treat cracked heels, it is recommended to consult with a podiatrist.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Dr. John Branwell from Kearny, New Jersey. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Kearny, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The Importance of Checking Diabetic Feet Daily
 Diabetes is a medical condition that often affects the feet. Elevated blood glucose levels can cause a lack of sensation in the feet, and existing cuts, bruises, and wounds may be difficult to notice. An untreated cut may lead to a diabetic foot ulcer, which may develop on the top or sides of the foot. It is important to check the feet daily, and to notice if there is swelling or a change in skin color. There are measures which can be implemented that may help to prevent the potential foot problems that are caused by diabetes. These measures can include controlling your blood glucose levels, wearing shoes that fit correctly, and avoiding walking barefoot. If you have diabetes, it is strongly recommended that you seek the counsel of a podiatrist who can help you manage your foot health.
Diabetes is a medical condition that often affects the feet. Elevated blood glucose levels can cause a lack of sensation in the feet, and existing cuts, bruises, and wounds may be difficult to notice. An untreated cut may lead to a diabetic foot ulcer, which may develop on the top or sides of the foot. It is important to check the feet daily, and to notice if there is swelling or a change in skin color. There are measures which can be implemented that may help to prevent the potential foot problems that are caused by diabetes. These measures can include controlling your blood glucose levels, wearing shoes that fit correctly, and avoiding walking barefoot. If you have diabetes, it is strongly recommended that you seek the counsel of a podiatrist who can help you manage your foot health.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. John Branwell from Kearny, New Jersey. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Kearny, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Conditions
Diabetes is the condition in which the body does not properly process food for use as energy. People with Type 1 diabetes cannot produce insulin, which is required for glucose to feed your body’s cells. It is typically caused by the immune system mistaking healthy cells for foreign invaders and destroying the insulin-producing cells in the pancreas. On the other hand, people with Type 2 diabetes cannot respond to insulin properly, and eventually cannot produce enough. The Centers for Disease Control and Prevention reports that over 30 million people in the United States have diabetes, with 1 in 4 having no idea they have it. Surprisingly, diabetes is the seventh leading cause of death in the US. The symptoms of diabetes include frequent urination, fatigue, hunger, and even blurry vision.
Diabetes can also affect the feet as well. Over time, diabetes can cause nerve damage to your feet, which could then lead to symptoms such as tingling, pain and numbness in the feet. Neuropathy can be very dangerous to a person with diabetes, since it prevents them from feeling injuries such as cuts or blisters in the feet, and if not detected early enough, may lead to infection. Neuropathy can also lead changes in the shape of your feet and toes. The best way for people with diabetes to prevent or delay neuropathy is keeping their blood glucose levels in their target range. This consists of eating right, having the correct amount of exercise, and taking medications.
Diabetes can also create calluses and foot ulcers as well. Calluses build up faster and occur more frequently with those affected by diabetes. If there are too many calluses, therapeutic shoes and inserts may be required. It is important to have calluses trimmed by a health professional, as doing it yourself may lead to infections. If these calluses continue to develop and thicken, they can lead to foot ulcers. Foot ulcers are open sores, that appear on the ball of the foot or on the bottom of the big toe. These ulcers can lead to future infections if not treated and may possibly result in losing a limb. It is important to report any ulcers to your podiatrist right away. Your doctor may take x-rays to examine the foot and clean out any dead and infected tissue.
Lastly, diabetes can also lead to poor circulation and peripheral arterial disease (PAD). The poor circulation in the feet and leg area is a result of diabetes narrowing and hardening, eventually slowing down the blood flow in that area. The best way to prevent this is to keep away from smoking and follow your doctor’s advice for maintaining blood pressure and cholesterol. PAD is similar to this complication. PAD is when blood vessels narrow or are blocked by fatty deposits. PAD also increases your risk of heart attacks and strokes and is a common condition to those affected by diabetes. The combination of both PAD and neuropathy may lead to infections and can result in amputation of certain limbs. PAD can be prevented with wearing the proper foot wear and regularly taking care of your feet.
If you want to take care of your feet, you should wash and dry them carefully and perform daily inspections to check for cuts, blisters, or swelling. Any physical activity you partake in should be approved by your health care provider. You should also be sure to wear special shoes if advised to do so by your doctor.
Runners May Be Prone to Stress Fractures
 Patients who enjoy running marathons are familiar with the possibility of getting stress fractures. They can happen as a result of increasing mileage and speed too soon and not warming up properly before running. A stress fracture is defined as a hairline fracture in the bones that can gradually develop over time. The symptoms that patients experience include pain, swelling, and difficulty walking. Additional reasons why this type of injury can occur include wearing shoes that do not fit correctly or frequently changing running surfaces. After a proper diagnosis is performed, which generally consists of having an X-ray taken, treatment can begin. Treatment options can include wearing a protective boot for approximately six weeks. If you have endured a stress fracture, please speak with a podiatrist as soon as possible.
Patients who enjoy running marathons are familiar with the possibility of getting stress fractures. They can happen as a result of increasing mileage and speed too soon and not warming up properly before running. A stress fracture is defined as a hairline fracture in the bones that can gradually develop over time. The symptoms that patients experience include pain, swelling, and difficulty walking. Additional reasons why this type of injury can occur include wearing shoes that do not fit correctly or frequently changing running surfaces. After a proper diagnosis is performed, which generally consists of having an X-ray taken, treatment can begin. Treatment options can include wearing a protective boot for approximately six weeks. If you have endured a stress fracture, please speak with a podiatrist as soon as possible.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact Dr. John Branwell from Kearny, New Jersey. Our doctor can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
- Gender – They are more commonly found in women compared to men.
- Foot Problems – People with unusual arches in their feet are more likely to develop stress fractures.
- Certain Sports – Dancers, gymnasts, tennis players, runners, and basketball players are more likely to develop stress fractures.
- Lack of Nutrients – A lack of vitamin D and calcium may weaken the bones and make you more prone to stress fractures
- Weak Bones – Osteoporosis can weaken the bones therefore resulting in stress fractures
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions, please feel free to contact our office located in Kearny, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
Who Can Trim My Toenails?
 The importance of taking care of your feet as the aging process occurs is crucial for possibly avoiding painful foot conditions. It is common that senior citizens have decreased circulation, and sores or wounds on the feet may take longer to heal. Many elderly people have difficulty trimming their toenails, and it often helps to see a podiatrist who can properly trim them on a frequent basis. Additionally, neuropathy is a common foot ailment among elderly people, and it can be difficult to feel existing bruises or cuts on the feet. If you are an elderly patient, it is strongly suggested that you are under the care of a podiatrist who can treat and prevent foot conditions.
The importance of taking care of your feet as the aging process occurs is crucial for possibly avoiding painful foot conditions. It is common that senior citizens have decreased circulation, and sores or wounds on the feet may take longer to heal. Many elderly people have difficulty trimming their toenails, and it often helps to see a podiatrist who can properly trim them on a frequent basis. Additionally, neuropathy is a common foot ailment among elderly people, and it can be difficult to feel existing bruises or cuts on the feet. If you are an elderly patient, it is strongly suggested that you are under the care of a podiatrist who can treat and prevent foot conditions.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Dr. John Branwell from Kearny, New Jersey. Our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Kearny, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Taking Care of Elderly Feet
Many foot diseases and conditions become more serious and common among the elderly. Some of these conditions include diabetic ulcers, ingrown toenails, fungus, arthritis, corns, and calluses. Unfortunately, it may be harder for older adults to take care of their own feet, but there are some precautions they can take in order to avoid any serious conditions.
Dry, cracked heels tend to be a common problem for older people. In order to avoid this, you should always keep your feet clean and well moisturized. Special feet moisturizers should be used as average lotions might not provide enough moisture for dry and cracked heels. Daily foot inspections are crucial for the elderly to detect any irregularities in their earliest stages. During the aging process, blood circulation tends to slow down causing older people to not feel their feet as well as they used to. This often results in foot problems going unnoticed.
Fungal and bacterial conditions thrive on elderly feet because older adults are less likely to keep their feet clean and dry; this makes it easier for bacteria to take hold in their dry, cracked skin. Elderly people should be sure to thoroughly dry their feet, especially in between the toes, after bathing. This will help them avoid developing any fungal infections. Additionally, clean cotton socks should be worn after the feet are dried.
Cutting toenails straight across will help prevent ingrown toenails. When toenails are cut too lose, the nail might break through the skin resulting in an ingrown nail. Clippers should be used to cut the nails in order to make the cut even.
Elderly people who have diabetes are at risk of developing serious foot problems that may lead to amputation. Ulcers that are left untreated can lead to gangrene. Dry and cracked feet, fungus, and untended cuts under the nails may also lead to infections.
Fortunately, Medicare covers many different types of services for foot care. Elderly people with any of these foot conditions should seek the help of a podiatrist and perform daily foot inspections in order to ensure that they have healthy feet.
An Overview of Morton's Neuroma
Morton’s neuroma is a condition that occurs when a nerve located near the base of the toes becomes compressed. This condition causes pain in the ball of the foot that has a burning quality and numbness that radiates to nearby toes. The pain from Morton's neuroma often increases while walking or when the ball of the foot is squeezed. Sometimes, the pain is severe enough to interfere with walking, leading to a limp. If you have symptoms of Morton’s neuroma, it is suggested that you see a podiatrist. A podiatrist can examine the affected foot, order diagnostic imaging tests, and provide treatment options.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. John Branwell of Kearny, New Jersey. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Kearny, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.